Sam Greenwald
MS, Public Health Administration & Policy (executive program)
Advisor:
Carrie Henning-Smith
Keywords:
Sexual and Gender Minorities, Health Communication
Abstract
Learning Objectives:
- Attendees will be able to describe the reasons that Minnesotan SGM give for choosing not to disclose SOGI data to their PCP.
- Attendees with learn to recognize traits related to patient demographics and healthcare utilization among Minnesotan SGM that are associated with disclosure of SOGI data to PCPs.
Background: The NAM and Joint Commission recommend collecting data about sexual orientation and gender identity (SOGI) to address disparities among sexual and gender minorities (SGM). However, barriers that SGM face in disclosing SOGI data to primary care providers (PCPs) require further research.
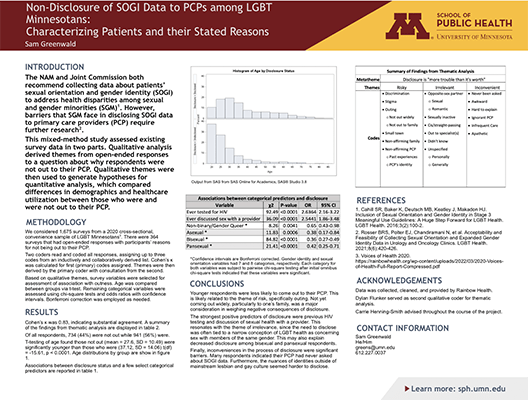
Methods: This mixed methods study conducted secondary analysis of 1,675 surveys from a 2020 cross-sectional, convenience sample of LGBTQ+ Minnesotans. For thematic analysis, we coded 364 open-ended responses describing reasons for not disclosing to PCPs. Qualitative themes were then used to generate hypotheses for quantitative analysis, which consisted of t-tests, chi-square tests, and odds ratios with confidence intervals comparing differences in demographics and healthcare utilization based on disclosure status.
Results: Qualitative analysis yielded three themes: that disclosure was perceived as risky, irrelevant, and inconvenient. One meta-theme also emerged: that disclosure is “more trouble than it’s worth”. Those not out were about 9 years younger than those who were out (27.76 vs. 37.12, t=-15.61, p<0.0001). Previous HIV testing (OR=2.64) and previous discussion of sexual health with a provider (OR=2.54) had the strongest positive associations with disclosure. Conversely, those who identified as non-binary/gender queer (OR=0.65), asexual (OR=0.38), bisexual (OR=0.36), or pansexual (OR=0.42) were less likely to disclose. Chi-square statistics and confidence intervals were significant at alpha=0.05 for all ORs reported.
Conclusions: Patient and provider education could facilitate communication to more accurately assess how disclosure may impact care. Such interventions should focus on SGM with less well-known identities.
Acknowledgements: Data provided by Rainbow Health. Dylan Flunker served as qualitative second coder.