A major global clinical trial has begun to test neutralizing monoclonal antibody treatments on adults hospitalized with COVID-19.
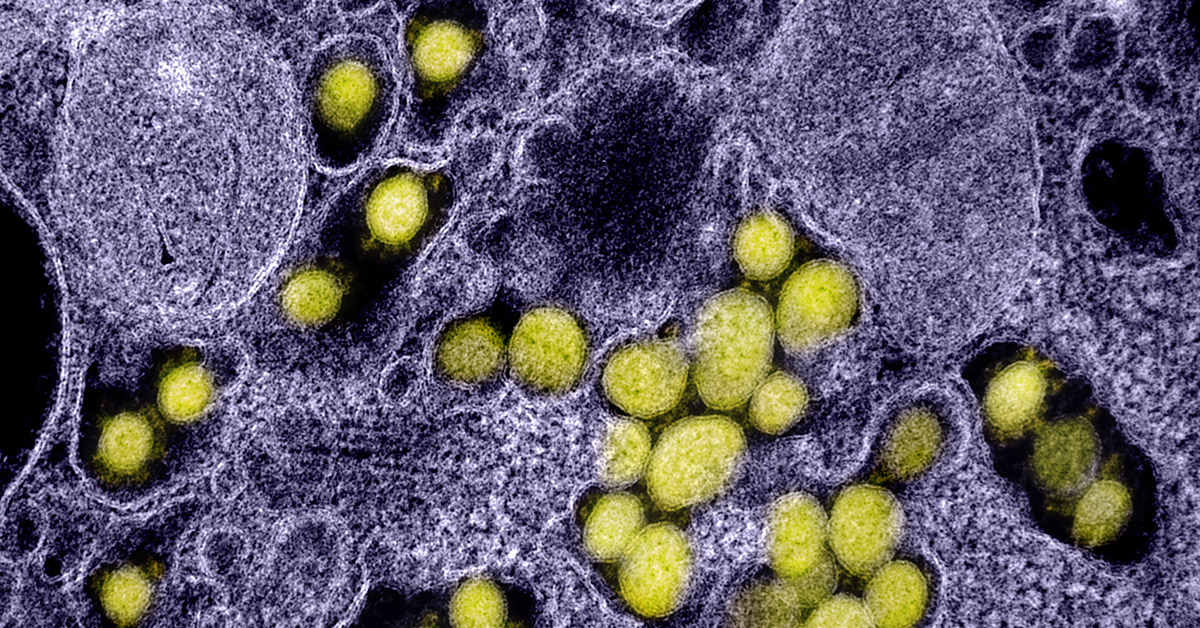
The antibodies used are synthetic versions of natural human antibodies. For use in this trial, antibodies specific to the virus that cause COVID-19 were singled out from the blood of recovered COVID-19 patients and then reproduced. When infused into people sick with the illness, the monoclonal antibodies will cling to the protein spikes surrounding the virus and keep it from infecting healthy cells, in effect, “neutralizing” it. The process may mimic what’s happening naturally in some young people and others who can handle the virus relatively well.
The first patient was enrolled in the trial on August 5, and others are quickly following in a study that will ultimately span hundreds of clinical sites around the world.
The study, called ACTIV-3, is part of the ACTIV (Accelerating COVID-19 Therapeutic Interventions and Vaccines) program at the National Institutes of Health (NIH) and is receiving support through Operation Warp Speed, a major effort by the U.S. government to fund, develop, manufacture, and distribute therapies and vaccines to fight COVID-19 as quickly and safely as possible.
The first neutralizing monoclonal antibody to be studied in the ACTIV-3 protocol is named LY-CoV555 and was developed and manufactured by Lilly Research Laboratories, Eli Lilly and Company, in partnership with Abcellera Biologics in collaboration with the NIH National Institute of Allergy and infectious Diseases (NIAID) Vaccine Research Center.
The ACTIV-3 trial will study the most promising neutralizing antibody treatments for COVID-19.
Four NIH-funded clinical trial networks with hospitals across the globe are carrying out ACTIV-3. The lead network is the International Network for Strategic Initiatives in Global HIV Trials (INSIGHT). INSIGHT is led by Professor Jim Neaton in the Division of Biostatistics at the University of Minnesota School of Public Health (SPH). The other networks, all U.S. based, are the Cardiothoracic Surgical Trials Network (CTSN); the Prevention of Early Treatment of Acute Lung Injury (PETAL) network; and the U.S. Department of Veterans Affairs.
“An advantage of the collaboration among the four networks is that hospitals can be activated to enroll participants in epidemic hot spots in the U.S. and around the world in order to more rapidly obtain answers concerning the safety and efficacy of the treatments to be studied,” says Neaton.
The ACTIV-3 trial will study the most promising neutralizing antibody treatments for COVID-19. A master protocol was rapidly developed to evaluate multiple treatments simultaneously or sequentially, and in early fall, the ACTIV-3 trial may expand to include three or four new treatments. Those may include polyclonal antibodies, which attack the virus from another angle.
ACTIV-3 is an adaptive 2-stage, randomized, double-blind, placebo-controlled trial. In stage 1 of the study, 300 patient volunteers will be assigned, at random, to receive either a placebo or LY-CoV555. All will be receiving the antiviral drug remdesivir as part of the study design. If LY-CoV555 appears safe and effective, based on intermediate short-term clinical outcomes, the trial will advance to stage 2 and an additional 700 patients will be randomized and enrolled.
The treatments will be evaluated by comparing the number of study participants in each randomized group who achieve sustained recovery, defined as discharge from the hospital and at home for 14 consecutive days. All participants will be followed for 90 days.
NIH chose INSIGHT to lead the ACTIV-3 trial because of its track record in conducting large, global trials on treatments for emerging infectious diseases. In addition to staff at the University of Minnesota, INSIGHT involves four international coordinating centers in Copenhagen, London, Sydney, and Washington, D.C., and more than 300 sites in 35 countries. The protocol chair for ACTIV-3 is Dr. Jens Lundgren, an infectious disease specialist, who also leads the Copenhagen center. INSIGHT is best known for the large HIV trials it has conducted (START and SMART) to establish the benefits of early treatment for HIV.
The INSIGHT leadership group and statistical and data management center is housed at the Coordinating Centers for Biometric Research (CCBR) in the Division of Biostatistics. CCBR, co-led by Neaton and Professor Cavan Reilly, includes several other faculty members from the School of Public Health and a faculty member from the U of M School of Statistics. Staff include a number of MS level statisticians, senior data management staff, and regulatory and safety specialists.
Over the last 30 years, CCBR, through INSIGHT and other NIAID/NIH supported work, has investigated treatments for HIV and influenza, and vaccines and treatments for Ebola, changing the way these diseases are managed across the globe.