A recent School of Public Health pilot study describes the results of a community health support worker program in a rural Ethiopian community aimed at improving retention in care by providing newly diagnosed HIV patients with health education, supportive counseling, and facilitated communication with their clinics.
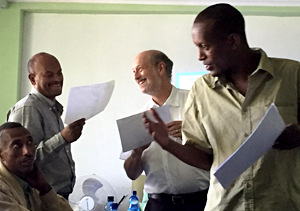
The program used local HIV-positive support workers who were selected, trained, and mentored by the program.
Overall, the research showed the program was associated with high rates of treatment retention among new patients attending HIV clinics, as well as improvements in HIV knowledge, physical and mental quality of life, and perceived social support, with reduced feelings of self-stigma.
The study was published in the Journal of the International Association of Providers of AIDS Care.
In Ethiopia, HIV-infected patients newly enrolled in care have the greatest support needs and risk of treatment default, with one study showing only 79 percent of patients continuing treatment after the first six months.
“Many patients defaulting from HIV care die without treatment or return only after developing advanced immune suppression and HIV disease,” says Alan Lifson, professor and lead author of the study.
Ethiopia, like many resource-limited countries, faces multiple challenges in providing care for HIV-infected patients, including lack of adequate numbers of trained health workers.
The study shows the use of community health support workers appears to help close this gap. Investigators found that after one year, 94 percent of new HIV patients were still retained in medical care.
Lifson and his colleagues are building on this research by initiating a new randomized community trial at 32 sites with over 2,600 patients throughout southern Ethiopia to further evaluate the impact of this community support worker program on retention in care and other outcomes for people living with HIV.